In the relentless pursuit of our fitness goals and the challenges posed by modern sedentary lifestyles, hip injuries have become an unwelcome companion for many. Whether you're a dedicated fitness enthusiast striving for a personal best or someone navigating the pitfalls of a desk-bound 9-to-5 routine, understanding and managing hip-related issues is crucial.
This article aims to shed light on the prevalent hip-related challenges faced by the average person and provide insights on how to tackle them independently. We'll delve into the signs and symptoms of hip joint and hip bone problems, empowering you to identify and address issues before they escalate. Moreover, we'll explore when it's prudent to seek professional help, ensuring you make informed decisions about your well-being.
Your hip joint: A quick overview
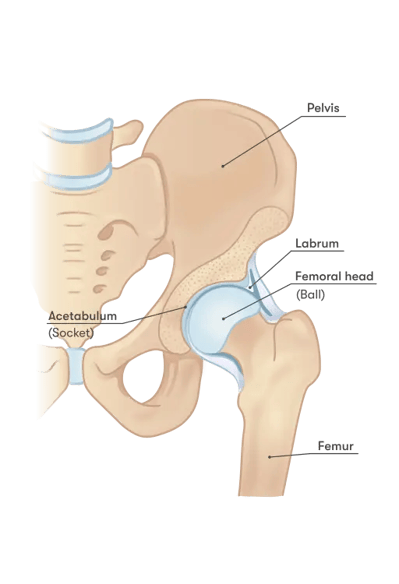
The hip is like your body's built-in hinge, letting you move around freely by sitting, standing, walking, running, and even jumping or hopping. Picture it as a superhero joint that can move in three directions – side to side, front and back, and twisting. It's pretty strong, thanks to tough ligaments and muscles that help keep things steady. Unlike the shoulder, which has a kind of flimsy joint capsule, the hip's capsule is a real team player in keeping everything stable. Think of it like a tight cover when you stretch your leg and a bit looser when you bend it. There's also something called a labrum, which is like a cushiony extension around the bony part of your hip. It's made up of tough collagen stuff and helps the thigh bone stay snug in its socket. So, your hip is a powerhouse that lets you move comfortably and smoothly.
Common hip problems or injuries we see in clinic:
- Excessive Anterior Pelvic Tilting or Lumbar Lordosis: Tilting your Pelvis too Much or Having a Super Curvy Lower Back
- Leg Length Discrepancies - LLD: Having One Leg a Bit Longer or Shorter than the Other
- Sacroiliac Joint Syndrome: Feeling Sore around the Joint Where Your Pelvis Meets Your Lower Back
- Hip/Femoroacetabular 'Impingements' (FAIs)
- Greater Trochanteric Pain Syndrome: Feeling a Bit Achy on the Outside of Your Hip
Hip Problem #1: Excessive Anterior Pelvic Tilting or Lumbar Lordosis
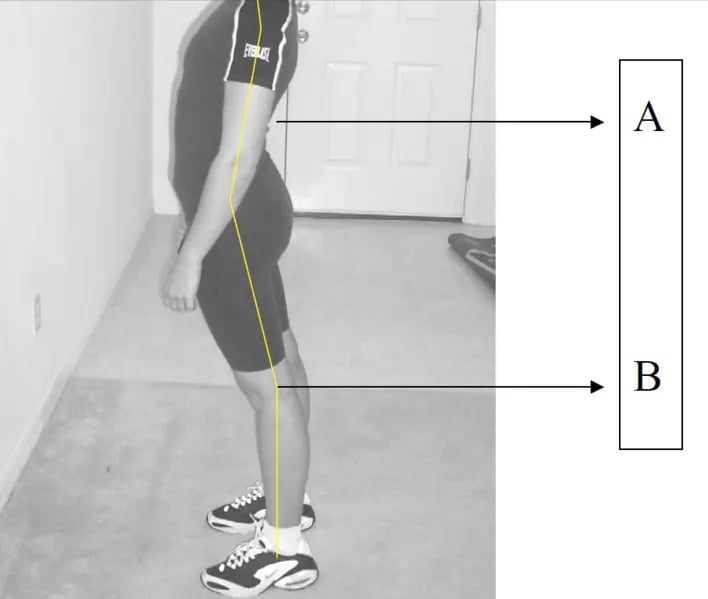 Lordosis. In a healthy posture, point A would be directly above point B
Lordosis. In a healthy posture, point A would be directly above point B
Excessive curvature of the lower back often with the chest outwards and hip pushed backward tends to have excessive spinal loading on the lower back.
Imagine your pelvis as a bowl. If you tilt it too much forward or if your lower back is super arched, it's like tipping the bowl too far forward. This can happen when you stand or walk, and it might make your lower back feel a bit strained. It's all about finding the right balance for a comfortable posture.
How to identify Excessive Anterior Pelvic Tilting
When you’re standing against a wall or lying flat on the ground, you’ll have a high arch (more than 1 hand width distance from the wall or floor).
How to “fix” Excessive Anterior Pelvic Tilting
Experts often suggest exercises like core stability, posterior pelvic tilting (basically, gently tucking in your tailbone), and abdominal strengthening. These exercises can help take some strain off your lower back and make you feel better.
Studies have found that folks with low back pain might not be super aware of their body positioning, especially around the pelvic area. So, these exercises aim to improve that awareness and help you move more comfortably.
Remember, while these exercises can be beneficial, they might not cover all the reasons for low back pain. If your pain sticks around or gets really intense, it's a good idea to chat with a professional first. They can guide you on whether these exercises are right for you and make sure you're managing the pain safely.
Hip Problem #2: Leg Length Discrepancies (LLD)

Leg length discrepancy is where one leg might be a bit longer or shorter than the other. It's not a big deal for most people, but it can sometimes lead to feeling a bit wonky when you walk or stand. It's like wearing shoes with different heel heights – it might throw you off a little, but it doesn't mean you can't keep going about your stuff. Overall, there are two categories of LLD:
First type of LLD: True LLD
An actual bony asymmetry exists somewhere between the head of the femur and the mortise of the ankle.
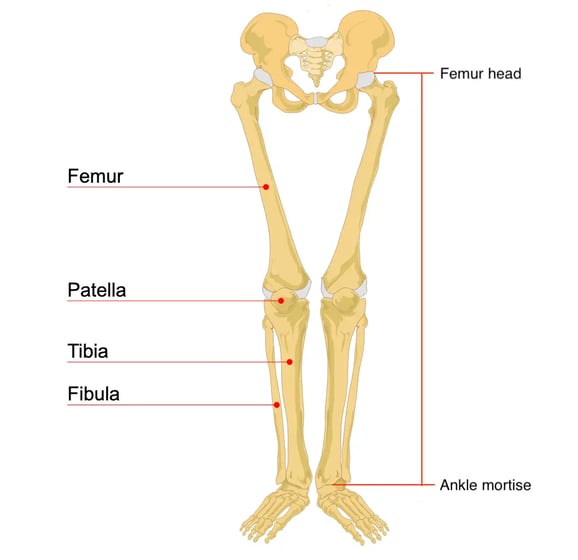
Sometimes, there's a natural unevenness in the bones between your thigh and ankle. This can happen for various reasons, like developmental quirks, fractures, injuries before your bones fully grow, degenerative issues, diseases like Legg-Calvé-Perthes, or even serious conditions like cancer or infections.
Legg-Calve-Perthes (LEG-kahl-VAY-PER-tuz) disease is a childhood condition that occurs when blood supply to the ball part (femoral head) of the hip joint is temporarily interrupted and the bone begins to die.
It's like your body's way of saying, "Hey, I'm a bit different on this side!" This unevenness can occur due to various factors throughout life, from growing up to facing certain health challenges. It's important to know that there's a range of causes for these differences, and it's not always something to stress about. If you suspect any concerns, it's wise to consult with a healthcare professional who can provide guidance based on your unique situation.
Second type of LLD: Functional LLD
A physiological response to altered mechanics along the kinetic chain anywhere from the foot to the lumbar spine gives the appearance of a short leg when a bony asymmetry in the length of bones might not exist.
Sometimes, your body reacts to changes in how it moves, from your foot up to your lower back. This can make it seem like one leg is shorter, even if the actual bones are pretty much the same length. It's like a domino effect – when something's off in how your body mechanics work, it can create an illusion of uneven leg length.
This illusion might happen because of things like soft tissues getting shorter, joints getting a bit stuck, ligaments being too loose, or even your body not aligning perfectly. Think of it as your body's way of trying to adapt to the way you move.
Foot mechanics can also play a role, especially if your ankle tends to roll in a bit too much. It's not always about the bones – sometimes, it's more about how everything else is working together. If you notice any concerns, talking to a healthcare professional can help figure out the best way to address these issues and keep you moving comfortably.
How to identify LLD
Measure your leg length with a measuring tape with the help of a partner/friend from the navel to the lateral malleolus (outer ankle) while standing.
Alternatively, you can do a quick check by looking at the popliteal fold line at the back of the knee and comparing heights between limbs and the height of the pelvis. This is to see if the differences are more thigh or shin-based.

How to “fix” LLD
If your uneven leg length is causing you some real hassle, here are some things you might consider. But remember, it's okay if you don't "fix" it unless it's causing significant problems.
First off, it's pretty normal for people to have some difference in leg length – about 70-90% of people have it to some degree, with 20% having a difference of more than 9 mm. Most of the time, these small variations don't cause major issues.
Now, when the difference is more pronounced, like above 20-25 mm, especially during active stuff like running or hopping, there might be more pressure on the shorter leg. This could lead to pain if your body isn't handling it well.
In such cases, seeing a podiatrist (a foot expert) might be helpful. They can suggest things like orthotics – fancy inserts for your shoes. Working with a physiotherapist could also be a good idea. They can check if your posture is playing a role and guide you on balancing things out.
Remember, sometimes issues in other joints, like your hips, back, knees, or ankles, could be part of the puzzle. Your body's a complex machine, and imbalances can happen.
In rare cases where the difference is severe, surgery might be considered. But don't worry, that's not the go-to solution for most people. Always consult with a healthcare professional to figure out what's best for you.
Hip Problem #3: Sacroiliac Joint Syndrome
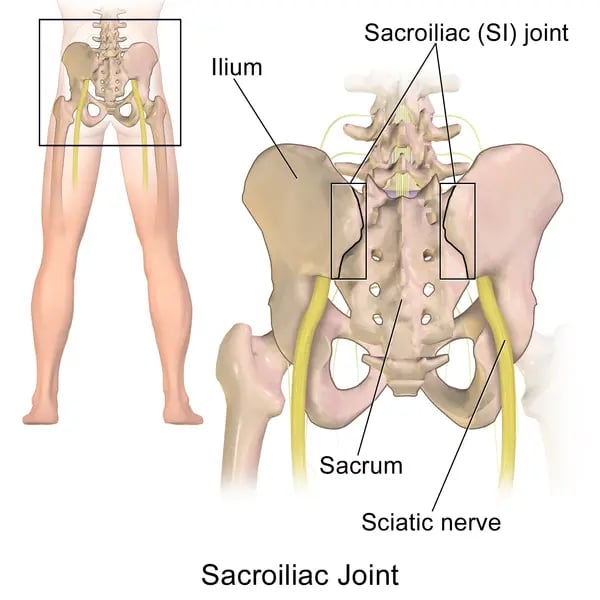
Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Sacroiliac Joint Syndrome is a term used to describe the pain of the Sacroiliac Joint (SIJ). The SIJ is the region where the sacrum meets the pelvis at the lower back region. It is usually caused by abnormal motion, being hypermobile or hypomobile, or any malalignment of the SIJ. Sacroiliac joint syndrome is a significant source of pain in 15% to 30% of people with mechanical low back pain (ref 3). Special note for those who are considered with Hypermobility Syndrome (check Beighton scoring with a Physiotherapist) and pregnant women due to increased relaxing hormones causing ligaments & other soft tissues to be more laxed to prep for the baby’s delivery.
Hypermobility means your joints can move beyond the normal range of motion. You may also hear the term double-jointed. This means your joints are very flexible. The most commonly affected joints are your elbows, wrists, fingers and knees.
Hypomobility of the SI joint refers to a decrease in the range of movement, inhibiting the ability to stretch normally. Hypomobility is often caused by arthritis, which triggers the bones to rub against one another and create extreme pain
Picture the joint where your spine meets your pelvis as a connection point. If it gets a bit irritated, you might feel some discomfort around your lower back or hips. It's like your body's way of saying, "Hey, take it easy around here for a bit!" It's usually nothing serious, but good to keep an eye on.
How to identify Sacroiliac Joint Syndrome
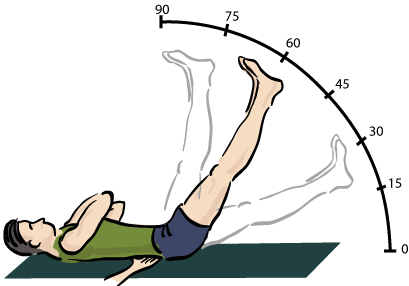
Pain at the lower back region during load shifting and single leg activities (i.e. standing on one leg, walking, jogging, running, stair climbing, etc) or during straight leg raise exercise (see image below).
How to “fix” Sacroiliac Joint Syndrome
Addressing core instability by activation and strength training. Proprioception training. Spinal & hip mobility exercises.
Activate and Strengthen Your Core:
This means waking up those core muscles and making them stronger. It's like giving your body's natural corset a little workout. Exercises that focus on your midsection, like planks or crunches, can do the trick.
Train Your Proprioception:
Proprioception might sound like a complex term, but it's all about your body's awareness of where it is in space. Think of it as your internal GPS. Simple exercises that challenge your balance, like standing on one leg or doing gentle twists, can help improve proprioception.
Embrace Spinal and Hip Mobility:
Keep your spine and hips happy with exercises that promote flexibility and movement. It's like giving them a little dance to do. Gentle stretches and rotations can make a big difference.
Hip Problem #4 : Hip/Femoroacetabular ‘Impingements’ (FAIs)
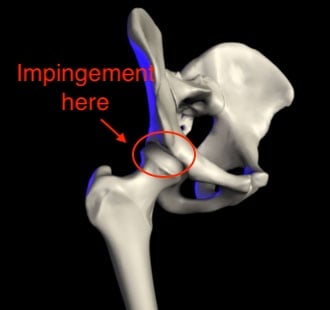
An abnormal bony shape and/or sizing of the femoral head-neck junction or the connections with the femoral head e.g. Cam and pincer hip morphology. These morphologies are thought to be fairly common (around 30% of the general population) (ref 4). including in people without hip symptoms.
Additionally, soft tissue or cartilage abnormalities may interfere with the regular mobility of the hip which may also contribute to and be a possible cause of femoroacetabular impingement (FAI). (ref 5)
There is a significantly higher prevalence of cam morphology in athletes compared to non-athletes. Cam morphology is more common in males than in females. A higher incidence of cam morphology has been found in high-impact sports e.g. football (soccer), hockey, American football, rugby, basketball, and baseball (ref 6). It is also linked with osteoarthritis of the hip: risk is 3-8 times higher than in non-athletes. (ref 7)
When your hip joint isn't moving as smoothly as it should, you might hear the term "hip impingement." It's like the bones in your hip are getting a bit too cozy, causing some friction. It's not a party for your hip, and it might lead to discomfort. Think of it like a hiccup in the smooth dance of your hip joint, but with the right moves, you can usually get things back on track.
How to identify FAIs
Xray investigation. When you notice that you have difficulty getting down into a deep squat (going past 90 degrees) or closely packed positions (flexion, adducted, internally rotated). Pain is usually specific to one location and usually deeper.
How to “fix” FAIs
If your hip issues aren't about bones and anatomy, here's a simpler approach to enhance flexibility:
Open Up Those Hips:
Think of your hip as a gate – you want to make sure it swings open smoothly. Work on extending your hip, moving it sideways (abduction), and turning it outward (external rotation). Simple stretches or exercises that mimic these movements can help.
Boost Hip Mobility and Stability:
Your hips are like the flexible center of your body, allowing you to move freely. Get them grooving with exercises that enhance mobility and stability. Picture it as giving your hips a little workout to keep them agile.
Seek Help from Physiotherapists:
If you want some expert guidance, consider reaching out to a physiotherapist. They can guide you through specific stretches, exercises, and even manual joint movements. It's like having a personal coach for your hip health.
Hip problem #5: Greater Trochanteric Pain Syndrome

The circled area is where you will usually feel the pain
Pain at the front hip or side of the hip like a twinge or dull ache on the side of your hip. This type of pain usually hangs out on the outer part of your hip and can happen for various reasons, from overuse to changes in your routine. It's a common issue, but there are ways to ease the discomfort and get back to moving smoothly.
How to identify Greater Trochanteric Pain Syndrome
Identify the problem by the location of the pain. You should look out for poor single-leg balance and Tredelenburg’s gait or hip drop in standing – pelvic tends to drop or fall towards an unsupported limb/side, and appears to be a waddling or catwalking gait. Or knee valgus (Knocked or inwards facing knee).
How to “fix” Greater Trochanteric Pain Syndrome
Hip mobility, stretching, and stability exercises. Commonly, good to work on strengthening the glutes (hip extensors, abductors). Walk or gait retraining.
If you're aiming for healthier hips without delving into the nitty-gritty, here's a straightforward plan:
Hip Mobility and Stretching:
Imagine your hips as doors – let's make sure they swing freely. Incorporate exercises that encourage hip movement and stretches to keep things loose. It's like giving your hips a gentle daily stretch to maintain flexibility.
Build Stability with Simple Exercises:
Stability is the key to happy hips. Strengthening your glutes, especially the muscles responsible for extending your hip and moving it sideways (abductors), can contribute to a stable foundation. Think of it as giving your hips a strong support system.
Strengthen Your Glutes:
Your glutes are like the powerhouse of your hips. Strengthen them by focusing on hip extensors (muscles that help your leg move backward) and abductors (muscles that move your leg away from your body). This is like adding a solid backbone to your hip health.
Retrain Your Walk or Gait:
Sometimes, it's all about how you move. Consider a bit of walk or gait retraining. It's like teaching your body to walk in a way that supports your hips better. Small adjustments can make a big difference.
Exceptions to look out for
While addressing hip conditions and injuries is crucial for overall well-being, there are instances where intervention might not be necessary or could be inappropriate. It's essential to consider individual factors and circumstances. Exceptions may include cases where the hip condition is minor and does not cause significant discomfort or limitations in daily activities. In some situations, attempting to "fix" a minor issue might outweigh the potential benefits.
Here’s a list of exceptions when the listed hip problems above should not be fixed:
For excessive anterior pelvic tilting or lumbar lordosis:
For those dealing with a tilted pelvis or lower back arch, don't feel pressured to fix it if you're not experiencing any pain or issues. Your body might have already figured out how to handle your daily activities and movements. Trying to overcorrect might lead to more discomfort, so sometimes it's best to let things be.
Leg Length Discrepancies (LLD)
Regarding differences in leg length (LLD) of 20mm or less, your body is pretty smart at adapting, and you might not need any special interventions. Don't stress too much about it unless it's causing significant trouble.
Impingements
When it comes to hip impingements, be cautious with the terminology – using words like "stuck" can create unnecessary fear. It might just be some discomfort or feeling a bit strained. It's important not to skip exercises altogether to avoid muscle weakening. X-rays might show things, but pain can come from various sources, not just bones or joints.
Greater Trochanteric Pain Syndrome (GTPS)
For Greater Trochanteric Pain Syndrome (GTPS), don't get too caught up in stretching and foam rolling for long periods. It's crucial to balance it with stability and strengthening exercises. If you've been focusing solely on massage and stretching, but the issues persist, it's possible the main cause, like strength or stability, hasn't been fully addressed. Consider consulting a physiotherapist to get a better understanding of what your body needs.
Conditions may be unique for each individual: best to seek professional help for effective treatment
In conclusion, it's crucial to understand that hip conditions vary significantly from person to person, considering unique anatomical structures and individual backgrounds. This article provides only a brief overview of common conditions, and the one-size-fits-all approach doesn't cut it when it comes to effective treatment. To ensure tailored strategies that address specific needs, seeking the guidance of a physiotherapist is highly recommended. Their expertise allows for personalized assessments, progression or regression of exercises based on individual capabilities, and the right treatment approaches.
Remember, attempting exercises without proper guidance can be risky, leading to potential aggravation of pain or condition. Therefore, if you're unsure or experiencing discomfort, it's always better to consult a professional for a thorough assessment. In cases of moderate to severe pain impacting daily activities, seeking immediate professional help is the best course of action for a swift and effective recovery. Your unique body deserves personalized attention, and a physiotherapist can provide the guidance needed for optimal hip health.
References:
- 1: Analysis of muscle activity during active pelvic tilting in sagittal plane by Sho TAKAKI. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342962/
- 2: Anatomic and functional leg-length inequality: A review and recommendation for clinical decision-making. Part II, the functional or unloaded leg-length asymmetry by Gary A Knutson. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1198238/
- 3: SLIPMAN W.C. Sacroiliac Joint Syndrome. Pain Physician. Vol. 4, N° 2, p 143-152, 2001. ISSN 1533-3159
- 4: Wall PD, Dickenson EJ, Robinson D, Hughes I, Realpe A, Hobson R, Griffin DR, Foster NE. Personalised Hip Therapy: development of a non-operative protocol to treat femoroacetabular impingement syndrome in the FASHIoN randomised controlled trial. Br J Sports Med. 2016;50(19):1217-23.
- 5: Trigg SD, Schroeder JD, Hulsopple C. Femoroacetabular impingement syndrome. Current Sports Medicine Reports. 2020 Sep 1;19(9):360-6.
- 6: Maupin JJ, Steinmetz G, Thakral R. Management of femoroacetabular impingement syndrome: current insights. Orthop Res Rev. 2019 Aug 27;11:99-108.
- 7: Feger J, Weerakkody Y, Knipe H, et al. Cam morphology (femoroacetabular impingement). Reference article, Radiopaedia.org (Accessed on 25 Aug 2023) https://doi.org/10.53347/rID-79706


.png?width=301&height=187&name=Website%20Navigation%20Images%20(3).png)

-1.jpg?width=1984&height=1196&name=UFIT%20Club%20Street%20Front%20(4)-1.jpg)






